State Farm is a large insurance company headquartered in Bloomington, Illinois. Its main lines of business include property and casualty insurance, as well as auto insurance. The company is the leading auto and home insurer in the United States.
In the 2023 Fortune 500 list, State Farm ranked 44th, showing its strong market position. According to its 2022 annual report, the company earned over $46.5 billion in premiums. However, it reported record underwriting losses – $13.2 billion – resulting in a net loss of $8.7 billion.
According to the most recent employment numbers (2019), the company employs approximately 58,000 people.
State Farm is proactively seeking innovative solutions, AI-based and otherwise, to gain an edge in a highly challenging and competitive industry. State Farm Ventures, launched in 2018 with $100 million in venture capital, appears to invest in tech-driven startups, including those that are AI-focused. The subsidiary invests up to $5 million per company, according to its site.
In this article, we examine two timely, relevant AI use cases that will be of interest to any insurance executive:
- Streamlined customer communications: AI-driven CRM and financial services platform empowers State Farm’s agents to quickly gather details about customers and craft personalized communications across channels, resulting in improvements to customer satisfaction, agent productivity and customer loyalty.
- Expedited contracts processing and analysis: Utilizing natural language processing, computer vision and machine learning to accelerate the contract analysis process, resulting in significant improvements to employee productivity and reduced costs.
- Combating insurance fraud: Using anomaly detection and predictive modeling to detect current fraud and to anticipate and counteract emerging threats in the insurance industry.
Use Case #1: Streamlined Customer Communications
Recent market studies repeatedly show that CX is crucial to financial and organizational outcomes in the insurance sector. For example, according to one study by McKinsey, insurance companies that delivered above-median “customer experience scores” outperformed their peers in terms of TSE, revenue growth and agent and employee satisfaction.
According to Salesforce, State Farm’s partner on this project, the insurer aimed to simplify its end-to-end customer experience across all customer contact channels – app, online and phone. To these ends, Salesforce reportedly combined its Financial Services Cloud product with Tableau CRM, an AI-based analytics platform.
Financial Services Cloud is a CRM solution that provides tools and features tailored to client business requirements (e.g., onboarding, financial planning, relationship management, etc.) Per a Salesforce commercial targeting insurance agents, Financial Services Cloud allows insurance agents to:
- Combine all desired business metrics in one place
- See customer claims, policies, premiums and renewals across each insurance type
- View financial account and household data
The short video below shows Salesforce’s value proposition to insurance agents:
The other half of the system, Tableau CRM – an end-to-end predictive and prescriptive analytics solution built for Salesforce – uses AI to provide data-driven insights and visualizations. As attested in the case study, Tableau CRM enables users to analyze large volumes of data, identify patterns and help make informed decisions. In the case of State Farm, Salesforce decided to combine the two solutions to enhance analytics capabilities in order to serve the customer better.
The short, two-minute video below shows how CRM Analytics provides intelligent insights for its end users:
The solution appears to be an integral part of the customer service workflow. We may reasonably infer, based on public information, that the customized system works as follows:
- The customer contacts State Farm by phone, online or through the State Farm mobile app.
- A comprehensive view of customer data is sourced from the Financial Services Cloud. This information may include their personal details, policy information, previous customer service calls and more.
- The information acquired from the customer data pulled in step two is analyzed by Tableau CRM. This analysis could involve pattern identification, customer segmentation, trend forecasting, claim resolution actions and more.
- The system produces visualizations, reports, or direct recommendations to the agent (including the prioritized to-do list).
Regarding business results, the case reports from both companies are not forthright with details. According to Salesforce, the new system simplifies the customer and associate experience and drives customer loyalty. No additional details were offered, however. It’s likely that State Farm also uses the integrated system to upsell and cross-sell its insurance products to existing policyholders.
However, given their losses in underwriting for FY2022 (as we stated in our introduction to this article, the net losses of which equalled roughly $8.7 billion), one would conclude that – as robust as the use case must be for State Farm – it is not enough to make up for the difference.
Use Case #2: Expedited Contracts Processing and Analysis
Understanding the relationship between risk and capital is a fundamental aspect of the insurance business, with contract management playing a pivotal role. When contract management is overlooked or substandard, it can cause several problems for insurers, including “lapses in insurance coverage, invoices with pricing that doesn’t match the contract, delivery delays and possible miscommunications” – as described in a report by the California Association of Public Procurement Officials.
As reported in an case report by Edgeverve, State Farm’s partner for this project, the insurer was grappling with several contract management challenges:
- A labor-intensive, lengthy process involving large teams of lawyers and subject matter experts (SMEs).
- Legal claims arising from noncompliance or alleged noncompliance with applicable laws.
- Difficulties in processing policy renewables on time.
- High expenditures due to fees paid to lawyers and SMEs.
In an effort to streamline the process, reduce time and costs and minimize potential errors, EdgeVerve reportedly integrated its XtractEdge product, an AI-powered Intelligent Document Processing (IDP) platform.
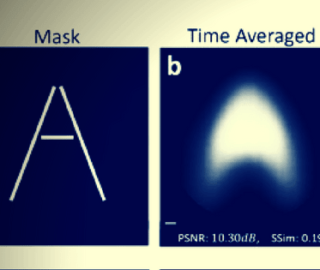
The product is designed to extract information from contracts using advanced machine learning techniques like computer vision and natural language processing. The video below provides an overview of the value proposition and some features of the XtractEdge Contract Analysis product:
Based on the features and capabilities of XtractEdge, we can infer the likely workflow:
- Document ingestion: StateFarm begins by inputting their contracts into the XtractEdge system in various formats such as PDFs, images, handwritten notes, etc.
- Information extraction: XtractEdge employs AI models to extract information using machine learning techniques like computer vision and natural language processing.
- Scoring and risk identification: The AI system scores the contracts based on predefined thresholds and identifies risky clauses that necessitate manual intervention.
- Digitization: The extracted information is digitized and made accessible for further analysis or action.
According to EdgeVerve, State Farm realized the following business results:
- 900% improvement in employee productivity.
- Approximately 90% cost savings during the contract review process.
- 90% less time spent on contract review.
The results suggest that AI can significantly enhance contact management in the insurance sector, potentially mitigating challenges like those faced by State Farm. However, it’s important to note that while AI can automate and streamline certain aspects of contract management, it does not eliminate the need for human oversight, expertise or intervention to ensure accuracy and compliance – especially in highly regulated industries like insurance.
Use Case #3: Combating Insurance Fraud
Insurance fraud significantly impacts companies like Allstate, with annual costs to the sector estimated at $308 billion, as reported by a Colorado State University Global study for the Coalition Against Insurance Fraud (CAIF). (Note: This figure may vary, with some estimates as low as $40 billion; however, the CSU-CAIF study suggests these lower numbers may not fully account for emerging fraud types or inflation adjustments. It’s advisable for interested parties to conduct further research.)
Perhaps the single biggest reason for the drastic increases in insurance fraud is the drastic rise of digitized claim filing. Fraudsters can open multiple policies and file numerous bogus claims across insurers and lines, according to a recent PAYMNTS interview with Greg Firestone, the VP of Data Science at Allstate. These statements would lead us to believe these two problems are of particular concern to the company.
A screenshot of State Farm’s insurance fraud reporting portal. (Source: State Farm)
To help curb fraud, Allstate claims to use an AI-driven fraud prevention system that analyzes multiple variables to determine the likelihood of a claim being false. AI-powered fraud prevention systems typically use machine learning algorithms to analyze various data points and patterns to assess the risk of fraudulent activity. The system may pull in multiple data points, depending on the type of claim filed. For example, in the case of a fire damage claim, the data may include:
- Claim history: Checks for past claims for any patterns of frequent or suspicious claims.
- Social media check: Scans public social media feeds if the claimant mentioned anything about travel or home issues that could corroborate his story.
- Weather reports: Cross-references the date of the claim with weather reports to ensure there were no environmental factors that could have prevented a fire, such as heavy rainfall.
- Financial stress indicators: Assesses financial background for signs of recent financial stress that might motivate a fraudulent claim.
While acquiring all of this data, the AI performs a statistical and machine learning-based technique called anomaly detection to identify patterns or instances that deviate from the norm. The system outputs a risk score that indicates the likelihood of a claim being fraudulent. The score helps Allstate’s claims adjusters prioritize which claims require further investigation.
Though specific business results are proprietary to Allstate and not publicly disclosed, AI-driven fraud detection systems have been shown to generally reduce false positives, increase detection rates of fraudulent claims and save on costs associated with fraud investigations. By improving the accuracy and efficiency of fraud detection, Allstate can protect its bottom line and maintain trust with its legitimate policyholders.
However, there are signs that – while State Farm’s AI-enhanced insurance fraud systems have been in place for at least the last two years – they do not function in a way that supports State Farm’s mission. According to a New York Times profile in December 2022, African American State Farm customers were seeking a class-action suit claiming that the insurance carrier discriminated against them.
The plaintiffs in the case presented a broad study to the court with critical data they claim shows that State Farm makes it more difficult for African American customers to get homeowner’s insurance claim payouts and how specifically the company’s fraud detection systems are directly to blame for the discrimination. According to Bloomberg, the plaintiffs won class-action status for the lawsuit earlier this year.
It is difficult to tell precisely the fiscal damage to State Farm’s bottom line from the poor publicity, not to mention the clear evidence that their fraud detection systems are not functioning in unity with the company’s core business goals. As the class-action lawsuit nears, that damage only stands to grow more widespread and more difficult to prescribe a tangible dollar amount.