
Although one might assume healthcare companies are investing the most amount of money into AI for R&D efforts, such as clinical trials, drug discovery, and surgical robotics, the top healthcare companies don’t seem to be publicizing their efforts if they are.
These could be for a variety of reasons, as we outline in our article How to Discover the AI Initiatives of Fortune 500 Companies, but we might assume it’s to prevent their competitors from garnering competitive intelligence on those companies.
Instead, it’s much more common to see healthcare companies advertising their AI initiatives for white-collar automation and business intelligence, and that’s certainly the case for McKesson, UnitedHealth Group, and Cardinal: three of the largest healthcare companies in the world.
In this article, business leaders can learn about the current AI initiatives and projects at these three top healthcare companies. We list some of their initiatives below:
- McKesson partnered with Genpact to allow for internal machine learning-based big data analytics and acquired Change Healthcare to offer healthcare companies white-collar automation such as contract management, order to cash, source to pay, and more.
- UnitedHealth Group’s Optum subsidiary offers the OptumIQ predictive analytics platform to healthcare companies with the promise of helping them forecast sales, market demand, and pricing accuracy.
- Cardinal Health offers predictive analytics for monitoring operations, estimating the resources patients might use and insurance claims management through its Vitalsource GPO service.
Our overview starts with McKesson and their AI initiative with Genpact for big data analytics.
McKesson
McKesson is a world leader in healthcare supply chain management solutions, health information technology, and oncology. The company is currently ranked sixth place in the Fortune 500.
Partnership with Genpact: White-Collar Automation
They have been improving their data management and analytics systems using machine learning since 2016 and partnered with Genpact to optimize numerous processes within their business, such as:
- Order to cash: customer sales orders for goods and services and payments for those orders, such as prescription drugs for patients or medical tools for hospitals.
- Record to report: collecting and delivering relevant and timely information. This could include telepathology and teleradiology information or a lab test where results may be communicated.
- Contract management: this could include automated reminders when contracts with supply companies or pharmaceutical companies could end. Analytics systems may also consider active contracts when recommending the best next step for the business leader to take.
- Master data management: the management of the company’s big data and how data is stored within the company. In healthcare, this mainly refers to patient EHR data that would be held in the client company’s database.
- Source to pay: the process of managing company spending and where funds can or should be allocated. This is essentially using predictive analytics to budget while considering patient data and possibly discerning future resource utilization by those patients.
Acquisition of Change Healthcare: Claims Management and Predictive Analytics
McKesson also acquired the AI firm Change Healthcare, which seems to have given them access to predictive analytics solutions for value-based care and reimbursement, or those services priced according to the value received by the patient. Change Healthcare’s machine learning-based analytics software could also assist McKesson with ensuring payment accuracy and improving revenue by reducing missed payments and chargebacks.
Claims Management Software
Most recently, Change Healthcare announced a solution called Claims Lifecycle Artificial Intelligence. The company added the software to its Intelligent Healthcare Network and its financial solutions in order to optimize claims processing for providers and payers. They claim the solution is made for optimizing the entire lifecycle of a claim, from when the claim is first filed to when it is paid or rejected.
According to the infographic from McKesson below, the software can detect claims that will be denied during the claims’ submission. The machine learning model would compare the claim to past accepted claims to verify its accuracy:
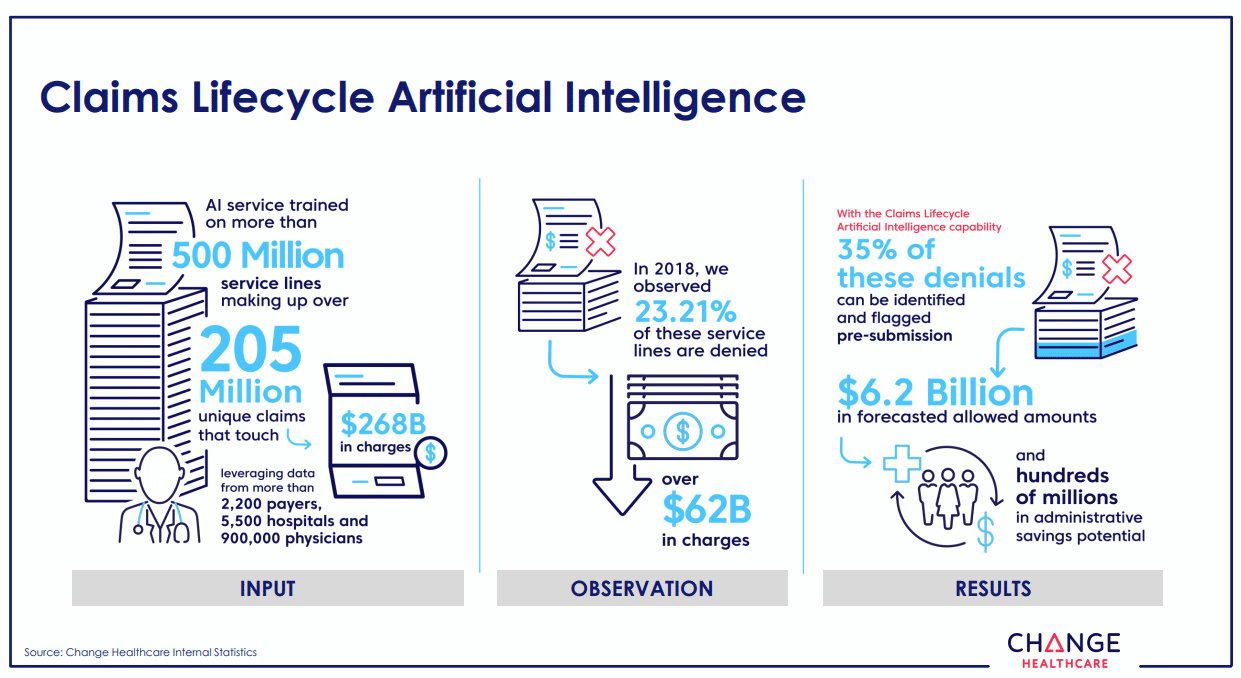
It might detect a claim that will be denied based on the signature on the claim or the amount the claim is for, among other criteria. Denying the claim could allow the claimant to complete any information they have missed or correct any inaccurate information themselves. This purportedly results in $6.2B in administrative savings across all of Change Healthcare’s clients.
Although there isn’t much information on the solution at this time, it is likely that the software uses predictive analytics to detect information within each claim and verify if it is correct and complete. We can infer this because Change Healthcare focused primarily on data analytics and predictive analytics before McKesson acquired it, in addition to the way in which Claims Lifecycle Artificial Intelligence seems to work.
Predictive Analytics Software
Change Healthcare offers an analytics platform called HealthQx, and the company claims it can help healthcare providers transition to value-based care and reimbursement using predictive analytics. Value-based care and reimbursement are required for healthcare providers under the Affordable Care Act (ACA).
HealthQx uses episodic claim grouping to detect the dates where rises in operational costs begin and end. It purportedly can then label this time period as an episode in order to focus specifically on a surge in costs to find the exact dollar amount for reimbursement.
This technique automates a process typically slowed down by human error. This could lead a healthcare provider to a lower reimbursement amount, which would mean lower revenue for the company as a whole. The predictive analytics portion of HealthQx can then use the data within each episode to find additional insights for future analytics projects. Change Healthcare calls this “episodic analysis.”
HealthQx’s machine learning model likely needed to be trained on hundreds of thousands of forms and records from the client healthcare provider, such as electronic medical records (EMRs), claims data, or financial data. All data would need to be relevant to company resources and operational costs, patient health and satisfaction, and items or services that can be reimbursed by the ACA.
It is likely that HealthQx also has a natural language processing (NLP) portion because EMR data typically contains unstructured data written in common language that NLP software could more easily parse.
We spoke with Daniela Braga, founder and CEO of DefinedCrowd Corp. about determining the data needs of an AI project, and importantly, what she wished executives knew to have a better grasp on what is required, reasonable, and possible with AI.
DefinedCrowd Corp. is a data collection vendor for AI projects and initiatives. The company offers services for training machine learning models on the appropriate data for their clients’ AI initiatives.
When asked for one important thing she could impart to her fellow executives, Braga said:
I think it’s important that more people understand what is high-quality data. Everybody talks about quality but most people don’t really care. A lot of offerings don’t measure quality. They have to understand that we have a certification for every data unit we produce or process. A lot of companies don’t do that and a lot of executives go by pricing instead of quality….That can hurt an organization’s project lifecycle. I’ve been there. It just delays everything and turns out to be more expensive in the end. That is to me the biggest pain…to pay attention, to not be fooled by the words and the buzz and look at the certification.
Once the company has selected the highest quality data sets they can prepare, a Change Healthcare data scientist or one from the client company would expose the machine learning model to all of this data.
This would train the machine learning model to correlate data points with opportunities for reimbursement, along with healthcare practices that lead to better patient outcomes at the population level. HealthQx could then make predictions about which operations will have reimbursement opportunities and which healthcare practices could use improvement.
McKesson and Change Healthcare claim their value-based care solutions are currently being leveraged by a number of health plan providers that cover a collective 33% of commercially insured citizens in the United States. That said, they do not mention any of these providers by name on their website.
Nick Giannasi is the Chief AI Officer of Change Healthcare, and he holds a PhD in Molecular, Behavioral, and Morphological Evolution from the University of Wales. Prior to his work at Change Healthcare, Giannasi served as Vice President of Life Sciences Product Strategy at Oracle.
UnitedHealth Group
Unitedhealth Group Inc. is one of the largest healthcare services companies in the world. They claim to offer services and solutions involving the organization of resources for local market demand and connecting all levels of healthcare through their technology.
Additionally, they claim to offer services for collecting, managing, and analyzing insurance enterprise data, including claims, electronic health records, and sales.
UnitedHealth Group serves its client companies and consumers from its two branches. The company provides healthcare coverage and benefits services from its UnitedHealthcare platform. For the consumer, this consists of a website where one makes an account and uses it to apply for healthcare or healthcare services.
The second platform is called Optum, which UnitedHealth Group acquired to provide information and technology-based services. Optum offers some machine learning-based data analytics solutions to health insurers, healthcare providers, and life sciences companies, and those solutions are powered by the company’s artificial intelligence platform called OptumIQ.
The machine learning software can purportedly leverage enterprise healthcare data to predict sales, market demand, and pricing accuracy for clients. In terms of market demand, the software would leverage past sales data along with any current market data the client company may have to upload into the system.
The software could then predict significant rises in demand, and if the client company used geolocational data, the software may also be able to determine where in the country the demand will rise.
It is most likely that the OptumIQ software has both a predictive analytics portion and a natural language processing portion. This is because Optum claims the software can analyze data from electronic health records (EHR), which contain unstructured data from physician notes that a natural language processing model could extract and detect data points from.
In addition to EHR data and healthcare provider notes regarding patient visits and their experience, Optum states the software is trained on structured data. This data includes data about a given hospital’s patient population and healthcare claims payment data.
Below is a graphic from Optum that highlights OptumIQ’s main components and capabilities:
According to a case study listed on Optum’s website, the company was able to help NYUPN measure how many resources their patients were using while they were cared for by hospitals and providers outside of their network. NYUPN is a collaboration between NYU Langone Medical Center and the University Physician’s Network.
NYUPN was purportedly able to build the necessary data reports they needed in order to have productive discussions with their physicians about their patients’ visits. Teaching the physicians about out-of-network utilization purportedly led to an increase of in-network utilization by 5% in one year.
In a video from Optum about their work with NYUPN, Executive Director Matthew Penziner had the following to say:
Optum performance analytics brings together clinical and claims data alongside socioeconomic data to support the best possible quality and cost outcomes. We have the flexibility to expand on built in analytics to surface additional data points, answer further questions, and create our own reports.
Matthew Versaggi is the Senior Director of Artificial Intelligence and Cognitive Technology at UnitedHealth Group. He holds a master’s degree in Computer Science with a specialization in artificial intelligence. Prior to his work at UnitedHealth Group, Versaggi served as an artificial intelligence engineer at Imagine One Technology and Management, Ltd.
Cardinal Health
Cardinal Health is one of the world’s leading distributors of wholesale pharmaceuticals and medical and surgical supplies. They distribute to hospitals, alternate care centers, chain drug stores, and supermarket pharmacies.
Numerous companies within the pharmaceutical supply chain rely on Cardinal Health’s services to transport their product to market. The company also offers machine learning-based data analytics solutions to pharmaceutical and healthcare companies for business intelligence purposes.
Cardinal Health’s Vitalsource GPO (group performance optimization) service is at the center of all of its machine learning solutions. They all leverage predictive analytics, and solutions that handle EHR/EMR data would also likely need to leverage NLP.
While most of these solutions are made for oncology, the company lists some of their solutions under urology and interdisciplinary cases. These are the CardinalHealth AI solutions covered by the Vitalsource GPO service:
- GPO Contract Dashboard: for assessing ROI and contract compliance
- Physician Dispensing: for organizing the pharma workflow and increasing patient compliance with medications
- Practice Analytics: for measuring, monitoring, and reporting on daily activities, as well as determining resource utilization and best practices for the hospital or healthcare provider.
- Regimen Analyzer: for estimating the total cost of care for a patient, identifying reimbursement opportunities, and making the most of drug spend.
- Remittance and Claims Management: for finding fair reimbursements and improving negotiations with payers with more transparency in important claims data.
- Jvion Cognitive Machine for Oncology Practices: a machine learning software from Jvion made for determining the best cancer care practices for individual patients. Jvion’s software is accessible with all of Cardinal Health’s own solutions from the Vitalsource GPO service.
According to a case study from Cardinal Health’s website, the company helped Tennessee Oncology manage their GPO contracts. They also claim to have helped Tennessee Oncology implement a new inventory management system for transporting oral and IV medications accurately.
“Data management will be the lynchpin for those who succeed,” said Jeff Patton, M.D. and CEO of Tennessee Oncology, “and you can’t do it on your own. As Cardinal Health Specialty Solutions continues to evolve into a data analytics company, they are well aligned with our needs.”
Tennessee Oncology was purportedly able to integrate oral and IV drugs into a single dashboard, which allowed for more visibility of spending and better reflected the numerous treatment options available for patients.
As more drugs become available for oncology, they will need to be better integrated into business models. Tennessee Oncology looked to address this with their solution, and claim to have found success with Vitalsource GPO.
Troy Zimpfer is the VP of Data Management and Analytic Services at Cardinal Health. He holds a Master’s Degree in Predictive Analytics from Kellogg School of Management. Prior to working at Cardinal Health, Zimpfer served as an executive consultant for The Scotts Miracle-Gro Company.
Header Image Credit: U.W. Marx







