Healthcare is an increasingly complex sector of the global economy, and AI is playing an active role in the worldwide evolution of the industry throughout its many disciplines. In a Deloitte study released earlier this year, 85% of respondents among healthcare business leaders said their enterprise was increasing AI spend before 2023.
Efficiencies created by AI applications and other technologies are anticipated to save $150 billion annually for the healthcare industry by 2026, according to a study last year from Accenture.
One area where AI is particularly well-suited to healthcare-specific business challenges of healthcare is the ability to process and transform large amounts of data into useful insights humans are not capable of articulating on their own.
As an example involving visual data, in particular, one recent study used an AI capability known as convolutional neural networks to analyze a large dataset of three-dimensional abdominal imaging from hospital patients. The researchers were able to identify organs-at-risk from hundreds of thousands of CT scans that would not have been detectable by human beings.
In harnessing the power of data, AI adoption across healthcare also stands to help patients identify a wider array of problems — from cancer to scoliosis — earlier than ever before. AI-supported technologies can help doctors provide more advanced care for patients, and improve efficiency throughout the entire healthcare system.
For example, imagine a patient who goes to the hospital for a routine checkup. Their vital signs are all normal, but the AI detects a slight change in their heart rate. The anomaly is flagged, and their doctor is notified. It turns out that the heart rate change detected by AI turns out to be an early warning sign of cardiac disease, and the patient can get treatment before it becomes life-threatening.
The list of relevant disciplines within the global healthcare space susceptible to AI application is equally long and continues to grow. In the following executive brief, we examine two prevalent AI use cases indicative of future adoption trends in healthcare:
- Diagnostics and visual data: healthcare providers are using machine learning and computer vision to absorb visual data and diagnose patients with increasingly rare conditions earlier.
- White-collar automation: AI also stands to streamline management workflows for non-emergency inventory (gloves, masks, general cleaning items).
Based on our research, we consider the trends that these use cases represent are behind exceptional economic and technological forces driving AI adoption in healthcare and describe them at length in the following summaries.
Afterward, we highlight three major obstacles holding back the industry from as rapid growth in industry-wide AI capability as we see in other legacy industries, like pharmaceuticals or banking:
- Privacy and Compliance
- Complex Stakeholder Dynamics
- Budgetary Constraints
Our summary of emergent healthcare use cases begins by taking a closer look at how visual and image-based data is the foremost driving force behind AI adoption among healthcare providers.
The Most Popular Use Cases:
Use Case #1: Diagnostics and Visual Data
Diagnostics are among the most popular use cases for AI applications in healthcare, both in machine learning and computer vision. Yet even among the entire diagnostics category, those use cases involving visual data and diagnostic information trend strongly as the most popular of the popular AI applications.
That popularity makes sense when one considers that imagery from MRIs and x-rays, in particular, is easy for AI to examine and offer diagnoses based on image qualities that it finds are indicative of specific symptoms.
- Diagnostics imagery is especially applicable to AI capabilities where they take place on mobile devices.
- Such is increasingly the case throughout healthcare to the point where the technology is believed to potentially help equalize patient outcomes across racial and socio-economic backgrounds.
- Given the ubiquity of visual diagnostics data, AI capabilities are applicable across conditions from colon cancer screenings to interventional radiology.
In the future, being able to connect image data with specific time and date information in the context of a patient’s larger health history and genetic information holds enormous potential in the hands of effective AI managers in the healthcare space.
(Source: U.S. Navy)
As Imagia COO and founder Dr. Alexandre Le Bouthilier notes in a recent AI in Business podcast episode, the problem in connecting these data forms is that they’re uniquely difficult for human beings to comprehend and find patterns as compared to machines:
“It’s very difficult for humans to understand fractal representation or even statistical patterns. So when we see something that has some statistical property, we can describe it but the machine will be able to do it,” Dr. Bouthilier explains.
The challenges in data presentation and perspective are similar for humans using artificial intelligence to find patterns in genetic information against very sensitive patient historical data. And of course, that’s before you even get to the challenges that ensuring privacy with patient data involves.
With the ability to advance human understanding and perspective from deficient two-dimensional imaging of genetic data, Dr. Bouthilier discusses how the impact of AI in the visual diagnostic space is akin to the invention of the microscope:
“The machines have come down to very low resolution… we see the microscopic effect of genetic mutation. And that, again, is difficult to capture from a human perspective. But the machine can certainly appreciate different patterns that are created by different genetic mutations…”
…So imagine for a second, you know that something is wrong because the doctor told you that the lesion is growing, but it’s still small. So we need to follow it up every three months until it doubles in size to make sure it’s really not that great before they go in for a biopsy. Sometimes this can take a year.
So imagine if you can do that, just at the first image, look at the image, and the computer tells something is wrong with that fixture, we should accelerate to the next phase of the cancer care continuum, and actually do a liquid biopsy for example.”
Use Case #2: White-Collar Automation
Whatever job someone has, they never want to admit that job can be automated. In healthcare, that means there are two sides to the automation equation.
- Healthcare providers dealing directly with patients and their very sensitive, protected information (i.e. doctors, nurses) hold AI largely at bay from their day-to-day workflows.
- Administrative workflows in hospital management for institutional tasks, not related to the Health Insurance Portability and Accountability Act of 1996 (or HIPAA) are not nearly as sensitive. — ensuring there are enough latex gloves in the hospital or that cafeteria equipment is replaced quickly enough so food service doesn’t suffer, as examples.
Thus, these latter functions are ripe for unmitigated AI application.
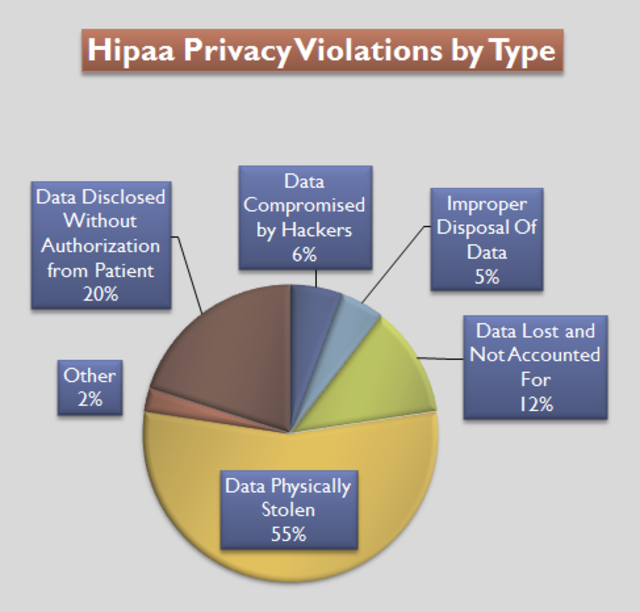
HIPAA Privacy Violations by the percentage of total violations for each violation type. Based on data available from The U.S Department of Health and Human Services for the period 9/22/2009 to 07/04/2012. (Source: Compliance and Safety LLC)
We will discuss more on why the former case of provider workflows and their application to AI adoption correlate directly to protections under HIPAA when we explore the barriers to AI adoption in healthcare later in this brief.
Where AI capabilities also stand to de-escalate costs and sensitivities in white-collar automation is in larger use cases of invoices and billing. Inherently, numbers- and language-heavy data from accounting in the healthcare space is similarly fertile terrain for AI.
There is another lesser-known yet remarkable benefit to the same already quite popular use case. Already across the healthcare sector, AI is making billing and debt collection more efficient by helping predict customers’ ability to pay based on past behavioral information.
In an interview on Emerj’s AI in Business podcast, CognitiveScale Executive Chairman Manoj Saxena explains how white-collar automation also means that debt payment collection operations can provide a more empathetic customer experience.
As Saxena details at length, it is a customer experience far more conscious of the correlations between a patient’s health history and their ability to pay for future care than ever before:
“The power of an AI is it can read structured and unstructured data, it can read an image, it can read a document, it can look at a complex ICD-9 claim structure. And the same goes for bad debts. So as you’re admitting patients, or as you’re treating patients to the process, the AI can look at a complete picture of both that particular individual and their capacity to pay, as well as individuals like that patient that you have dealt with in the past.”
By tracking patterns in payment history alongside other forms of healthcare data simultaneously, call agents can more acutely recommend payment programs and other benefits to patients in need. Potentially confrontational debt collection processes are instead approached with new evolving best practices, informed by what’s most likely to settle collections as quickly and efficiently as possible.
The Greatest Barriers to AI Adoption in Healthcare:
Privacy and Compliance
Ultimately, privacy and compliance concerns in healthcare depend on what’s called the privacy rule in HIPAA. Collecting the sheer amount of patient health data necessary for AI adoption is widely viewed as implicating HIPAA and associated state laws.
In December 2018, the near quarter-century-old law was born into the digital age when the Department of Health & Human Services Office Of Civil Rights (OCR) asked stakeholders in public healthcare policy to help the agency identify security weaknesses in HIPAA’s current policies.
The American Medical Informatics Associationh took the occasion as an opportunity to update HIPAA in light of emerging digital age technologies like AI, asking OCR for new requirements such as the timely sharing of protected health information between consenting patients and requesting clinicians.
The ensuing exchange shows providers and business leaders are caught between two competing interests in public policy deriving from HIPAA and subsequent revisions:
- The legal mandate to provide state-of-the-art care that protects patient data
- The business and organizational need to keep up with new technologies that increasingly require information without restrictions
The latter assures AI adoption trends in healthcare will grow at a pace determined by how subsequent use cases can work around HIPAA and other regulations.
Complex Stakeholder Dynamics
Stakeholders in the healthcare space are a source of tremendous complication and conflicting interests, as we discussed with white-collar automation and privacy concerns.
In a strictly economic sense, stakeholder dynamics are based on:
- Who buys a good/service
- Who benefits from the good/service
- Who uses the good/service
In the healthcare space, these stakeholders include:
- Hospital business leadership
- Doctors, nurses, medical staff
- Patients
Just as public institutions and professional associations have tremendous problems resolving differences over sharing private data efficiently, hospitals also balance the increasing influence of doctors, nurses, and administrative staff seeing technology increasingly entrench itself amid the near-sanctified relationship between patient and provider.
However, human providers aren’t alone in wanting to protect their jobs. Patients themselves are not enthusiastic about the notion of being treated by any kind of machinery to the apparent exclusion of empathetic oversight. No matter what the data tells us about the promise of AI and other advanced healthcare solutions over human capabilities, people trust other human beings with their health first and foremost in 2022. For the time being, healthcare business leaders have no choice but to compromise with their united front.
Budget Constraints
Operating efficient hospitals and healthcare facilities is about effective management of resources, above all being budgets. Though budgetary forces can drive AI interest, especially in areas we have described in white-collar automation, documentation, and the fact of the matter is hospitals do not have extra revenue to throw around.
According to a 2020 survey of healthcare business leaders by the American College of Healthcare Executives, 76% responded that budgetary fears held back their enterprise from further AI investment in that fiscal year.
The entire environment makes it much more difficult for champions to get the necessary buy-in for an AI project to succeed:
- AI investment requires early enthusiasm for exploration along with the long-term strategy and budget to let those mistakes not just become knowledge ROI but ultimately transform an enterprise.
- As enterprises, hospitals and healthcare management are traditionally much more short-term focused and usually staffed with former doctors with sanctified beliefs about the human connection between doctors and patients.
Thus we anticipate that AI adoption in the healthcare space, despite widespread opportunities and innovation in the short term, will not frequently advance long-term, organization-wide transformations in healthcare as AI does for relevant, image and language-heavy legacy sectors like banking or pharmaceuticals.



















